Fall Education and Prevention Campaign Helps Seniors Stay Safe and Independent
Someone’s “first fall” can end up being their last and devastating to their quality of life. It can end mobility as they know it and can quickly transition a spouse or child into a caregiver role. Annually, falls are reported by one-third of all people 65 and older and two-thirds of those who fall will fall again within six months. Falls are the leading cause of death from injury among people 65 or over.
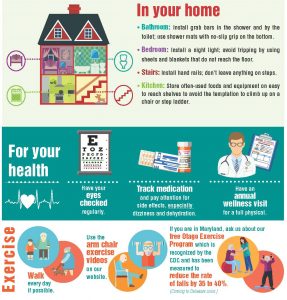
“One of the very first steps our team takes when visiting a new patient is a home assessment,” said Nancy Bagwell, area director of operations for Peninsula Home Care. “We know people want to be home to recover from their illness or injury but we need to make sure home is as safe and comfortable as possible. The last thing they want is to fall trying to get from their living room to the bathroom and end up back in the hospital. We look for fall risk factors such as area rugs and loose cords and want to make sure they have proper lighting for moving around their home safely.”
Fall prevention is critical for seniors and can help them lead a safer and healthier life. Knowing the more common risk factors for falls is critical to prevention.
Top Five Fall Risk Factors
1. Vision
Age-related vision diseases can increase the risk of falling. Cataracts and glaucoma alter older people’s depth perception, visual acuity, peripheral vision and susceptibility to glare. These limitations hinder their ability to safely negotiate their environment, whether it be in their own home or in a shopping mall.
Prevention Tips
• Have regular checkups by an ophthalmologist to discern the extent of age-related eye diseases such as cataracts and glaucoma.
• Use color and contrast to define balance-aiding objects in the home (e.g., grab bars and handrails).
• Add contrasting color strips to first and last steps to identify change of level.
2. Medication
Sedatives, anti-depressants, and anti-psychotic drugs can contribute to falls by reducing mental alertness, worsening balance and gait, and causing drops in systolic blood pressure while standing. Additionally, people taking multiple medications are at greater risk of falling.
Prevention Tips
• Know the common side effects of all medications taken.
• Remove all out-of-date medications and those no longer in use.
• Have a physician or pharmacist conduct a “brown bag” medicine review of all current medications.
3. Balance
Your balance gets worse as you age. Adding balance exercises into your physical activity can help.
Always hold onto a chair or table when with one hand when trying a new balance exercise. As you improve, you can just rest your fingertips on the table or chair. Also, have someone next to you when doing balance exercises for the first time – the person can help steady you or catch you if you fall.
4. Lack of physical activity
Failure to exercise regularly results in poor muscle tone, decreased strength, and loss of bone mass and flexibility. All contribute to falls and the severity of injury due to falls.
Prevention Tips
Engage regularly (e.g., every other day for about 15 minutes daily) in exercise designed to increase muscle and bone strength, and to improve balance and flexibility.
Undertake daily activities in a safe manner, such as reaching and bending properly, taking time to recover balance when rising from a chair or bed, learning the proper way to fall, and learning how to recover after a fall.
Wear proper fitting, supportive shoes with low heels or rubber soles.
5. Environment
At least one-third of all elderly falls involve environmental hazards in the home. The most common hazard for falls is tripping over objects on the floor. Other factors include poor lighting, loose rugs, lack of grab bars or poorly located/mounted grab bars, and unsteady furniture.
Prevention Tips
Conduct a walk-through of your home to identify possible problems that may lead to falling. A home visit by an occupational therapist might is helpful because they are trained to identify risk factors and recommend appropriate actions.
About Peninsula Home Care
Providing care for more than 30 years, Peninsula Home Care, in Salisbury and Ocean Pines/Berlin, Maryland, ensures that all patients are involved in their plan of care and strives to give them every opportunity to maintain their independence in the home. The agency has served more than 39,000 patients on Delmarva and was designated as a Peninsula Regional Medical Center preferred home care provider in 2017. For more information, visit www.peninsulahomecare.com.




